Category: Mental Illness
By Laurie Little, PsyD
Lindner Center of HOPE, psychologist
Depression can occur at any age. It does not discriminate. However, recent research suggests that young adults are experiencing symptoms of depression at higher rates than ever. There are many theories about why this is so, including the proliferation of social media, consequences of the Pandemic, escalating costs of living and even global issues.
Major Depressive Disorder is a result of a complex interplay of biological, psychological, and environmental factors. One’s family history, genetics, brain chemistry, life experiences, and stressors all contribute to its onset and severity.
However, there are unique challenges that young adults face that make them potentially at higher risk for experiencing depression. Young adults are trying to make their transition from dependency on parental figures and family support systems, to relative independence. There are new pressures that they are trying to manage that can be new and often confusing. There are academic, occupational, social, and financial pressures that can lead to feelings of inadequacy. Some young adults are woefully unprepared for the new responsibilities in their lives. They are also faced with transitions in their identity and being required to ask themselves questions about their life goals, meaning and purpose. These questions and challenges can all lead to anxiety, overwhelm and hopelessness when things are not going as they had expected.
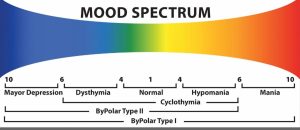
Recognizing the signs of severe depression in young adults is crucial for early intervention and support. Symptoms often manifest as sadness, however some young adults experience more irritability and an overall moodiness. There may be changes in appetite or sleep patterns, withdrawal from social activities, and even reckless or impulsive behaviors. A comprehensive assessment from a licensed health professional is required to make sure that depression is the only issue. Oftentimes, depression can co-occur with other mental health concerns such as anxiety.
Navigating conversations about depression with young adults requires empathy, patience, and understanding. Here are some helpful tips to facilitate meaningful dialogue and support:
Create a Safe Space: Establish an environment free of judgment where young adults feel comfortable expressing their thoughts and emotions. Avoid dismissing their experiences or offering unsolicited advice. Instead, listen actively and validate their feelings. (Example: “Of course you would feel upset about that, that sounds really difficult.”)
Normalize Mental Health: Foster open and non-judgmental discussions about mental health and addiction within your social circles and communities. By reducing the stigma surrounding depression, you empower young adults to seek help without fear of judgment or discrimination. Remember, everyone knows someone who struggles with a mental health issue or addiction.
Educate Yourself: Stay informed about depression and its symptoms in young adults. Empower yourself with knowledge about available resources, treatment options, and support networks.
Encourage Professional Help: While offering emotional and practical support is essential, it’s equally important to encourage young adults to seek professional assistance from mental health professionals. Provide information about treatment options such as psychotherapy and medication management, emphasizing that seeking help is a sign of strength, not weakness. Research is clear that the “Gold Standard” of treatment for depression is a combination of both therapy and medications.
Be Patient and Persistent: Healing from depression is a journey marked by ups and downs. Be patient with young adults as they navigate their emotions and experiences. Offer consistent support and encouragement, reminding them that they’re not alone in their struggles.
Psychotherapy for young adults is often a crucial step in recovery. Depression has been shown to be reduced by Cognitive-behavioral therapy (CBT) and mindfulness-based interventions. Family therapy may also be useful if the young adult is still living at home. Pharmacotherapy may also be required. For some young adults with treatment resistant depression (has not responded to traditional talk therapy or antidepressant trials) they may need to explore other treatment modalities, such as transcranial magnetic stimulation (TMS) and ketamine assisted therapy. These treatments offer new hope for individuals resistant to traditional treatments.
In addition to professional interventions, lifestyle modifications play a crucial role in managing depression. Encourage young adults to prioritize self-care activities, such as regular exercise, healthy eating, adequate sleep, and stress management techniques. Engaging in hobbies, creative outlets, and social interactions can also foster a sense of purpose and belonging. Be a healthy role model for the young adult in your life by trying to do the same.
Lastly, peer support groups and online communities provide valuable opportunities for young adults to connect with others who share similar experiences. These platforms offer a sense of solidarity and validation, reinforcing the message that recovery from depression is possible with the right support and resources.
Severe depression in young adults is a multifaceted challenge that demands a holistic approach to understanding, intervention, and support. In order to combat these rising rates, it is essential that we all work together to reduce the stigma of seeking help for depression and all mental illnesses and addiction. We must be vigilant about mental health symptoms in ourselves and our loved ones. Lastly, it is imperative that we provide empathy, support and resources when needed.
If you or someone you love is in need of mental health assessment or treatment, call the Lindner Center of HOPE at 513-536-HOPE or visit lindnercenterofhope.org for more information.