Author: pricilagran
 Paul Keck, MD Acknowledged in Psychiatry Category
Paul Keck, MD Acknowledged in Psychiatry Category
MASON, Ohio – Lindner Center of HOPE, a leading provider of mental health care, is pleased to announce that Paul Keck, MD, Psychiatrist in Chief and Founding President and CEO Emeritus, Lindner Center of HOPE, was named among Top Doctors 2023 as published in Cincinnati Magazine. He was selected by peers in a survey asking them which physicians they would turn to for care. The survey was conducted by Professional Research Services Company of Troy, Michigan.
Dr. Keck was one of only 10 physicians named in the psychiatry category, among a total of 869 physicians recognized in 68 specialties.
Dr. Keck has conducted extensive research in bipolar disorder and clinical psychopharmacology, supported by grants from the NIMH, NARSAD, the Stanley Foundation, the Marriott Foundation, and industry. Since 1996, he has been in the top 10 of the most cited scientists in the world publishing in the fields of psychology and psychiatry.
A magna cum laude and Phi Beta Kappa graduate of Dartmouth College, Dr. Keck received his MD with honors from the Mount Sinai School of Medicine, New York, NY. He served his internship in Internal Medicine at the Beth Israel Medical Center in New York and completed his residency training in Psychiatry at Harvard Medical School and McLean Hospital, Belmont, MA. Dr. Keck remained on faculty at McLean and Harvard before joining the Department of Psychiatry at the University of Cincinnati in 1991.
Dr. Keck is the author of over 400 scientific papers in leading medical journals. He has also contributed over 200 reviews and chapters to major psychiatric textbooks, and is the editor or author of 6 scientific books.
Dr. Keck is the recipient of numerous honors including being listed among The World’s Most Influential Scientific Minds by ScienceWatch.
About the Lindner Center of HOPE
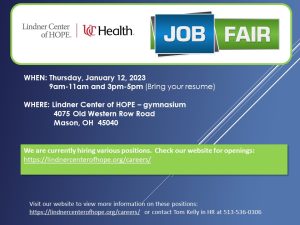
Lindner Center of HOPE in Mason is a comprehensive mental health center providing patient-centered, scientifically advanced care for individuals suffering with mental illness. A state-of-the-science, mental health center and charter member of the National Network of Depression Centers, the Center provides psychiatric hospitalization and partial hospitalization for individuals age 12-years-old and older, outpatient services for all ages, diagnostic and short-term residential services for adults and research. The Center is enhanced by its partnerships with UC Health and Cincinnati Children’s Hospital Medical Center as their clinicians are ranked among the best providers locally, nationally and internationally. Learn more at https://lindnercenterofhope.org/.