Category: Mood Disorder
For more than two decades, Screening for Mental Health has developed programs to educate, raise awareness, and screen individuals for common behavioral and mental health disorders and suicide.The vision is a world where mental health is viewed and treated with the same gravity as physical health, and the public’s participation in National Depression Screening Day helps make that vision a reality.
National Depression Screening Day, held annually on the Thursday of the first full week in October, is an education and screening event conducted by hospitals, clinics, colleges, and community groups nationwide. Much like the medical community screens for diabetes and high blood pressure, the goal is to offer large-scale mood disorder screenings for the public. The program provides free, anonymous screenings for depression, generalized anxiety disorder, bipolar disorder and posttraumatic stress disorder, as well as referral to treatment resources if warranted.
This year, October 8th, will mark 25 years of this revolutionary event.
Please participate in this milestone National Depression Screening Day and help spread the word to increase awareness of mental health. Take a screening now at http://screening.mentalhealthscreening.org/#/lindner-center-of-hope and encourage your family, friends and colleagues to do the same.
General
- Up to 80 percent of those treated for depression show an improvement in their symptoms generally within four to six weeks of beginning treatment. (NIH)
Global
- According to the World Health Organization, depression is projected to become the second leading contributor to the global burden of disease by 2020
- Depression is a common mental disorder. Globally, more than 350 million people of all ages suffer from depression. (WHO)
United States
- One in five 18 to 25 year olds experienced a mental illness in the past year
- An Estimated 1 in 10 U.S. Adults Report Depression (CDC)
- Major depressive disorder is the leading cause of disability in the U.S. for ages 15-44. (World Health Organization, 2004)
Physical & Mental Health Connection
- One-third of individuals with a chronic illness experience symptoms of depression
- People with depression are 4 times as likely to develop a heart attack than those without the illness.
- Many conditions may coexist with depression. Depression may increase the risk for another illness, and dealing with an illness may lead to depression. In fact, according to the NIMH, depression affects:
- More than 40 percent of those with post-traumatic stress disorder
- 25 percent of those who have cancer
- 27 percent of those with substance abuse problems
- 50 percent of those with Parkinson’s disease
- 50 to 75 percent of those who have an eating disorder
- 33 percent of those who’ve had a heart attack
- Depression is a prevalent and increasingly recognized risk factor for both the development of and the outcome from coronary artery disease (CAD). (National Institute of Health)
Depression is a treatable mental health disorder that causes persistent sadness and loss of interest. Some of the most common signs and symptoms include:
- Changes in sleep and appetite
- Poor Concentration
- Loss of energy
- Loss of interest in usual activities
- Low self-esteem
- Hopelessness or guilt
- Recurring thoughts of death or suicide
For a complete list visit: NAMI.org
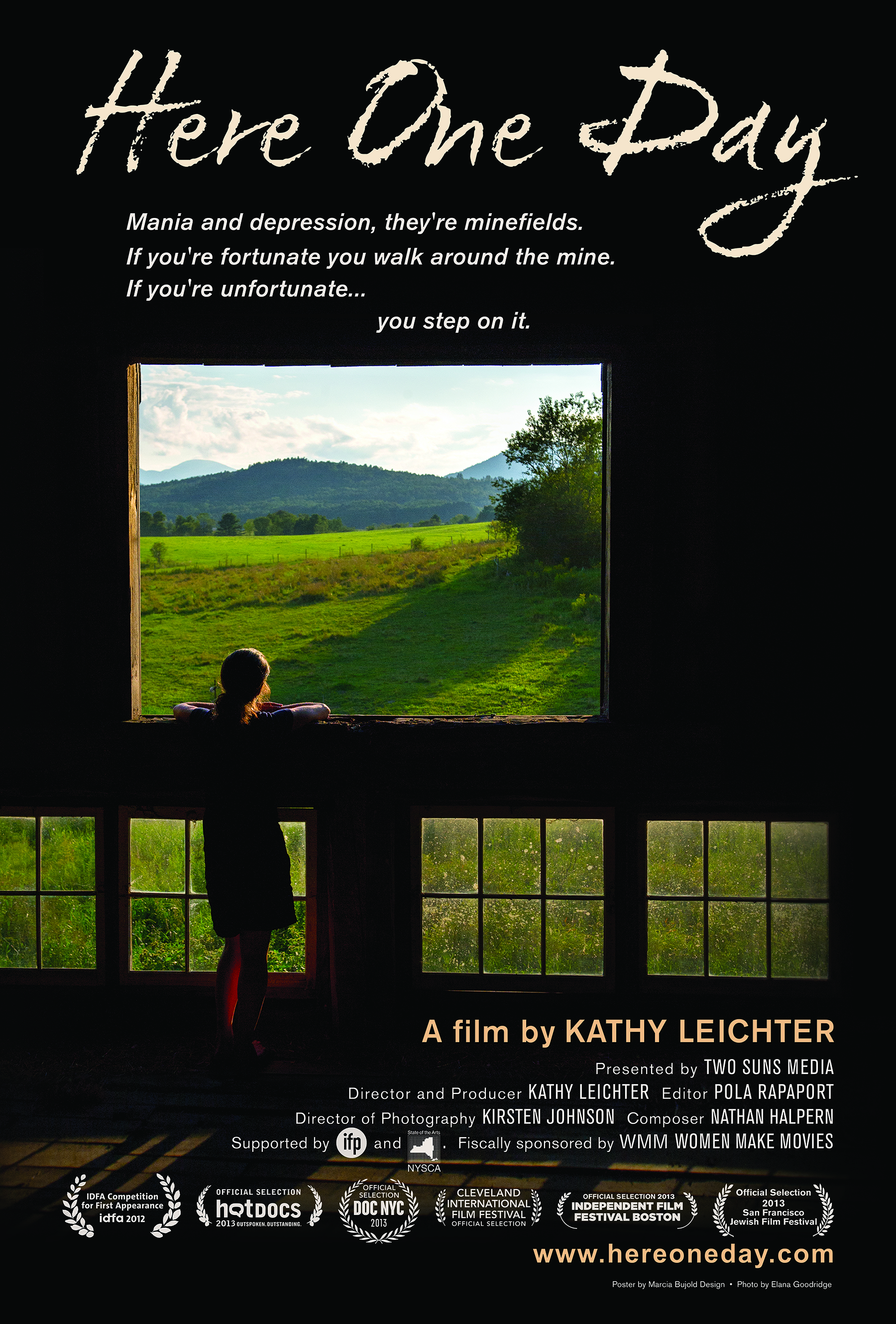
Bipolar disorder, also known as manic depression, is a treatable illness defined by extreme changes in mood, thought, energy and behavior. These changes are categorized into manic (high) and depressive (low) episodes, ranging from bursts of energy to deep despair. Some of the most common symptoms include:
Mania Symptoms
- Heightened mood, exaggerated optimism and self-confidence
- Excessive irritability, aggressive behavior
- Decreased need for sleep without experiencing fatigue
- Racing speech, racing thoughts, flight of ideas
- Impulsiveness, poor judgment, easily distracted
- Reckless behavior
Depressive Symptoms
- Changes in sleep and appetite
- Poor Concentration
- Loss of energy
- Loss of interest in usual activities
- Low self-esteem
- Hopelessness or guilt
- Recurring thoughts of death or suicide
For a complete list visit: dbsalliance.org
Generalized anxiety disorder (GAD) is an anxiety disorder that involves chronic worrying, nervousness, and tension. Some of the most common symptoms include:
- Feeling like your anxiety is uncontrollable; there is nothing you can do to stop the worrying
- A pervasive feeling of apprehension or dread
- Inability to relax, enjoy quiet time, or be by yourself
- Difficulty concentrating or focusing on things
- Avoiding situations that make you anxious
- Feeling tense; having muscle tightness or body aches
- Having trouble falling asleep or staying asleep because your mind won’t quit
- Feeling edgy, restless, or jumpy
For a complete list visit: helpguide.org
Posttraumatic Stress Disorder (PTSD) is a mental health condition that’s triggered by witnessing or experiencing a traumatic event. Some common symptoms include:
- Intrusive, upsetting memories of the event
- Flashbacks (acting or feeling like the event is happening again)
- Nightmares (either of the event or of other frightening things)
- Avoiding activities, places, thoughts, or feelings that remind you of the trauma
- Feeling detached from others and emotionally numb
- Difficulty falling or staying asleep
- Irritability or outbursts of anger
- Hypervigilance (on constant “red alert”)
For a complete list visit: helpguide.org