Author: pricilagran
Kaila Busken, Lindner Center of HOPE, Licensed Independent Social Worker
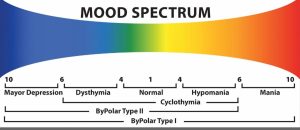
One moment you are bursting at the seams with overwhelming joy. Every fiber of your being is filled with love for this tiny human being in your arms. Looking in your baby’s eyes, you feel like you have found your life’s purpose. And still, motherhood is really hard. New motherhood is sitting in the messy middle of seemingly opposite feelings. You can feel a mixed bag of emotions: sad and happy, overwhelmed, and peaceful, grief and joy, lost and found.
The transition to motherhood and its ambivalence has its own name: matrescence (pronounced like adolescence). The term was first developed by medical anthropologist Dana Raphael in 1973. This term is used to describe the bio-psycho-social- spiritual change that occurs when a woman makes the transition to motherhood. Like in adolescence, matrescence is a physical, hormonal, and emotional change all happening at the same time. Matrescence recognizes the large shift in identity that occurs when a woman becomes a mother and helps to normalize what it feels like to be in the middle of a whirlwind of emotions. Motherhood is a magical metamorphosis, because once you have a baby, nothing will ever be the same. And that is both beautiful and sad.
Around 15-20% of women who birth a child will experience postpartum mood disorders such as depression and anxiety. But matrescence is a normal part of motherhood and it is normal to feel ambivalence in this season of life.
Here are some helpful tips for coping in this new season of life:
1. Let go of expectations.
From the time a woman decides she is going to have children she hears an influx of information about what it means to be a mom and how to care for her baby. One of the biggest things a mom may hear is “you don’t have time for yourself anymore.” An important thing to remember is that you are a person worth caring for. You deserve to eat. You deserve a hot shower. You deserve to hydrate yourself. And you deserve love. You may even have a “Pinterest” perfect image in your head of what motherhood would be like. You may have pictured a blissful bubble in which you only feel complete happiness, but it is important to allow yourself to embrace the messiness and imperfection that is motherhood.
2. Build your support system.
Just as a baby was born, you as a mother were born too. It is okay to ask for help and it is important to find a group of people who will help care for you. Look for people who will help support you emotionally while you adapt to your new role. Also look for people who will provide practical support like doing that pile of dirty dishes in your sink or the endless pile of laundry that babies create. Babies are tiny but they certainly require a village.
3. Practice self-compassion.
Being a new mother is difficult. Suddenly this new little life is depending on you day and night and it can be exhausting. It can be easy in this new vulnerable state to be harsh and self-critical. During this time, it is especially important to practice self-compassion and remind ourselves of our own worth. It can be easy to believe that you are a “bad” mother and that you are not providing what your baby needs. An important self-compassionate reminder is that “you are the best mother for your baby”. The goal is not for you to be a perfect mother but rather to be a “good enough” mother and embrace all the imperfection that comes with raising a baby. Perfection in motherhood is not possible and practicing self-compassion can help in remaining resilient in the face of this new role.
4. Embrace the ambivalence.
Motherhood is embracing so much of the messy middle between seemingly opposing emotions. It can be uncomfortable to be in this place, where you want to spend every moment with your precious newborn and to crave the independence and space you had prior to having a baby. Motherhood is about the “both/and”, knowing that good and bad can exist in the same place. It is possible for you to embrace them both at the same time. You can love your baby with every fiber of your being and miss a time when you were able to sleep through the night or drink a hot cup of coffee.
5. Allow yourself to grieve.
It is okay to grieve in this new phase of life. We tend to believe that grief is only reserved for death, but we can grieve many things in this new phase of motherhood. You may grieve your old life, previous relationship dynamics, your body and how it may have worked before, your time, your envisioned birth plan, your envisioned feeding plan, or your expectation of what you thought motherhood would be like. Allowing yourself to feel the sadness in some of these losses will help you to move on and embrace your new role as a mother.